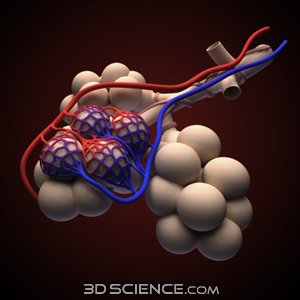
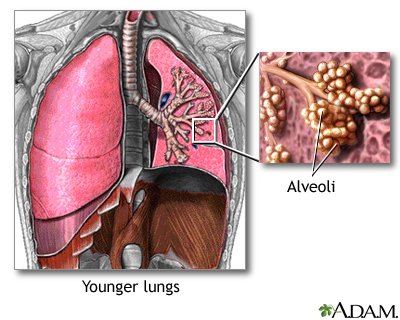
Pulmonary edema refers to extravasation of fluid from the pulmonary vasculature into the interstitium and alveoli of the lung. The formation of pulmonary edema may be caused by 4 major pathophysiologic mechanisms: (1) imbalance of Starling forces (ie, increased pulmonary capillary pressure, decreased plasma oncotic pressure, increased negative interstitial pressure), (2) damage to the alveolar-capillary barrier, (3) lymphatic obstruction, and (4) idiopathic or unknown mechanism. Cardiogenic pulmonary edema (CPE) is defined as pulmonary edema due to increased capillary hydrostatic pressure secondary to elevated pulmonary venous pressure. CPE reflects the accumulation of fluid with a low-protein content in the lung interstitium and alveoli, when pulmonary veins and left atrium venous return exceeds left ventricular (LV) output.
Increased hydrostatic pressure leading to pulmonary edema may result from many causes, including excessive intravascular volume administration, pulmonary venous outflow obstruction (eg, mitral stenosis or left atrial myxoma), or LV failure secondary to systolic or diastolic dysfunction of the LV. CPE leads to progressive deterioration of alveolar gas exchange and respiratory failure. Without prompt recognition and treatment, patients' conditions can deteriorate rapidly.

 akhi
akhi