covering the topic of nephrology today:
figure out what kidney is failing?
______________
your approach:
renal failure has three main causes
pre-renal azotemia .. kidney not to function not because the problem is in the kidney rather in the circulation.
the second is intra-renal azotemia, or intrinsic renal disease--
and the third is post renal azotemia
problem with inflow to the kidney, or the outflow being blocked or can have disease within the kidney.
Now we start with pre-renal azotemia:
pre-renal many think of as dehydration, it is true in part, but it is a problem that is caused by poor perfusion, cause occur from dehydration and volume depeltion, or lost fluid from burn, third spacing during pancreatitis, or bad burn, kidneys aren't getting enough blood flow in, can have also cardiovascular disease, hypotensive because of poor cardiac output, not enough circulation to the kidney will be read as poor blood volume. inadequate blood to the kidney.
the same thing can happen if you have a situation of low albumin level leading to decreased oncotic pressure, like in nephrotic syndrome or cirrhosis, dec. intravscular volume because they run a low vascular volume. Kidney thinks it isn't getting enough blood.
the final main cause, is overt circulatory problem, like narrowing of renal artery, stenosis. Or medication induced vasconstriction, NSAIDS for instance, some of the blood flow is prostogandin dependent. cause the kidneys not to function and cr. goes up.
these are the causes of pre-renal. Not enough blood flow and not just because of dehydration.
why is pre-renal azotemia important. Important, conceived of as ischemic situation, if stays untreated, it will progress to where the kidneys necrose.
what you'll need to do is tell pre-renal from intra-renal because treatments are completely different.
________________
Next post renal, outflow problem
1- outflow of bladder can be obstructed, tumor in pelvis, scarring, strictures, BPH, back pressure goes back to kidney, causing obstruction of outflow..
or at level of ureters, stones, tumors, papillary necrosis, also putting back pressure unto the kidneys.
significance is back pressure on kidneys and damage
_______________
intra renal failure.. problem with the integrity of kidney, the most complicated of the three kinds..
intrinsicrenal, often acute tubular necrosis are many names due to kidneys not working.
how do you distinguish:
specify tests or lab data to interpret:
tests for post renal azotemia
first prostate exam, obstructed urethral outflow.
the best test however, check for residual urine in the bladder, have them urinate put catheter or scan with bladder scan to see how much urine is left after they urinate, typically they should only have 50cc or less
the best of all is an ultrasound, that looks at ureters, bladder.. which will detect hydronephrosis
now pre-renal azotemia
bunch of tests, the most widely used, is the ratio of BUN/CR
Cr level of 1
BUN 10
BUN more than 10 more than 30 it is a good indication of pre-renal
so that is a key labtest
the other more accurate
is measurement of urine sodium or fractional excretion of sodium
if kidneys are in a pre-renal situation , the kidneys say I am not getting enough blood, they think you're bleeding to death, so when they think that will, start retaining sodium to keep vascular volume, so urine sodium will be very low. short term treatment is fluids
urine sodium less than 10 is low
other things, same principal.. kidneys will also concentrate urine, high specific gravity and high urine osmolalaity, they are corroboratory findings.
typical case.
62 yr old for nausea and vomiting
his crt is 3.6 was normal 3 months ago, he also has orthostatic hypotension
BUN 82
urine sodium 6
specific gravity 1.028
BUN is more than 20:1
kidneys trying to replete vascular volume.. faced with this, this is pre-renal azotemia.
rx: fluids
_______________
intra-renal will see the opposite
BUN/CR is normal not elevated 10:1 or even less
will see instead of low urine sodium it will be high, because the kidneys are failing, they start leaking, so high levels of urine sodium
only place that falls down is pt who is on diuretic, so the test then loses value.
look for low BUN/CR
look for sodium spillage in urine
urine specific gravity and osmolality is low
you might also see red blood cell casts or granular casts, the kidney is falling apart and pieces of it coming apart, released into urine.
algorithm: approach to Azotemia
1- faced with high creatine level first thing you want to do is to exclude pre-renal azotemia :
a- what is the BUN/CR if >20:1
b-Urine Sodium <10
c-FeNA <1
d-OSM >300
f-specifc gravity > specific gravity rising by.001 for every 35 to 40 mosmol/kg increase in osmolality. Thus, a urine osmolality of 280 mosmol/kg (which is isosmotic to plasma) is usually associated with a specific gravity of 1.008 or 1.009. so higher than those values and now you know how to calculate 'normal'
sounds like pre-renal
if pre-renal is the case, then treat the cause, whether volume depletion, renal artery stenosis or heart failure..
also need to exclude post renal, using sonogram and post void residual urine, if see hydronephrosis then treat obstruction with stent etc
if no evidence or pre or post renal, then the problem is intra renal
BUN/CR not high
urine sodium that is high more than 20 or more than 30, FeNA that is greater than 1 and osm less than 300 and urine specific gravity is low since urine can't concentrate since kidneys aren't working properly.. that will tell you intrarenal ..
intrarenal failure there are many causes:
but they will either occur in the tubules and interstitum and the other occur in glomeruli which is glomerulonephritis ...
main categories:
first category and most important is ATN
acute tubular necrosis ..
occurs in different settings.. the tubules start falling apart, for instance in prolonged ischemia (shock kidney) hypotensive, labs look pre-renal but then kidney falls apart.. prolonged above conditions, clots of A fib, occluding renal artery...
2nd which are also common are toxins like
radiological contrast, drugs like amonoglycosides and amphotercin B, pigments like myoglobin from muscle breakdown
ATN occurs in phases, prodromal period of time
from beginning of insult to effect on kidney..
then when you have outright ATN, stop making urine, drop to nothing or 2cc an hr (oliguric) then there will be a diuretic phase of ATN
metformin with contrast are at a great risk..
another category is acute allergic interstitial nephritis, an allergy to a drug.. common drugs cephalosporins, beta lactams, methcillin hence we don't use it, sulfas, allopurinol
acute allergic nephritis, takes offending drugs, they'll get fever, rash, high eosinophil count, especially in the urine.
rx steroids short term
other tubulointersistial disorders
deposition disease, any number of chemicals can get into kidney, like hemoglobin is hemolyzed and out in circulation can deposit, myoglobin from rhabdomylisis, rx with high flow fluid to keep from crystalizing.
pts with Multiple myeloma crystalize Bence John's proteins
or crystalization of crystals, like oxalate, ethylene glycol antifreeze, part of mechanism of toxicity, is oxalate crystals depositing in kidney, also vitamin C in very big doses, can cause stones and crystalization.
crystalization of uric acid, for any disorder, like someone with lymphoma and it breaks off giving out uric acid, also in gout as well.
hypercalcemia, hyperparathyroid and crystallize calcium in the interstitum etc etc.
other causes of tubular interstitial disorders, infections like pyelonephritis, develop intrarenal, with white cell casts in urinary sediment.
others drugs and toxins, various analgesics NSAIDs, antibiotics.. outdated tetracycline.
variety of cancer deugs, cisplatin, mitomycin, methotrexate etc.
radiation nephritis, heavy metal poisoning...
glomeruldisorders
vasculitis type disorders (not very common) like wegner's granulamtosis
disorder with granulomatous dz in lung, paransal sinuses who also get lesions in the kidneys, intrarenal failure, high sodium in urine, cr high, problems with chronic sinusists and nasal congestion, maybe lesion in the lung as well.. test here is ANCA
Henoch shcnolen purpura, thrombotic thrombocytopenic purpura, htn etc.
other glomerular disorders, glomuerlonephritis, post streptococal glomerulonephritis.. get hypertensive and edema
do ASO titer to prove that the glomerulonephritis in someone who had a sore throat== post streptococoal glomerluonphritis
IGA nephrpathy, deposition of IgA following a viral illness...
chronic, like with collagen vascular dz. like SLE, also goodpasture syndrome
antibodies against basement membrane and lungs, will show up with intrarenal failure, and they will have lesions in lung and cough blood. order antibasement membrane antibodies
another Alport renal failure with hearing failure.
___________________________________________________
Now, how will we decide who has what...
glomerulonephritis
high urine sodium >20
High fractional excretion of sodium >1
BUN/CR suggesting not pre-renal
urinalysis will be key
hematurea and RBC casts = glomerulonephritis
most definitive tests to prove Glomerulonephritis is a kidney biopsy
things that go along with glomerulonephritis is nephrotic syndrome, also occurs in vascuilitis..
1- massive proteinurea massive 3.5 g 4+ dipstick positive and more
they lose intervascular oncotic pressure and develope edema, will run albumin down and hyperlipdemia
best test for nephrotic syndrome is a 24hr urine protein
best test to determine the type of glomerulonphritis causing this nephrotic syndrome is a biopsy.
some nephrotic syndrome are treated with prednisone
best first test (initial test) in a pt. with high urine sodium and indicators of intra renal failure.. is urinalysis!!!
infection, drug hypersensitivity, glomerulopnephritis, nephrotic syndrom, meyloma, uric acid (gout) and myoglobinurea.
what do we see in each of these?
infection= WBC and bacteria
pyelonphritis WBC casts
Drugs/ eosinophillia
glomuerlonephritis = RBC casts
Nephrotic syndrome = Hyperlipedmia, heavy protenurea
Multiple myeloma _ proteinurea
uric acid = uric acid crystals
Myoglobinurea = High CK levels and dipstick positive test for blood but no blood cells.
a different way
pyuria = infection
RBC casts = glomerulonephritis test with kidney biopsy
blood urine dipstick but not micro = myoglobinurea
crystals in uine = gout
eosinophils = allergic drug reactions
massive proteinurea = nephrotic syndrome
__________________________________________
cases:
62 yr old nausea vomiting, creatinine is 3.6 was normal 2 months ago, takes no meds
has large prostate, pulse is high, BUN is 72, urine specific gravity is 1.023
urine sodium = 9
all else is WNL
best initial rx..
likely cause.. he has a large prostate gland, potential outflow obstruction
tempted to get sono to measure post void.
his other things.. BUN 72 and cr 3.2 ratio of 20
concentrated urine
urine sodium of 9
all point to pre-renal azotemia
best initial rx is fluids
_____________________
case II
62 yr old nausea vomiting. CR 3.6, taking NSAIDS
labs
urine specific gravity 1.004 dilute
BUN 41/ 3.6 almost 12:1 ratio
urine sodium = 42
renal problem spilling sodium, can't dilute urine even though dehydrated, he has renal disease, with many dx to consider..
what is next? do sonogram to exclude post renal azotemia, then go back and say renal dz and work it up.
________________________
boy with high BP, edema, urinalysis, proteinurea and RBC casts..
young boy with glomerulonephritis.. blood test to do is ASO titer.
__________________________________
ESRD
end stage renal disease
renal failure that is incompatible with survival..
need dialysis or kidney transplant
how does it show up?
chronic findings and acute findings
important points, need for dialysis isn't determined by creatinine
hypocalcemia
kidneys are supposed to make 1.25 hydroxy vitmin D, because they are not working, you don't have this chemical so don't absorb calcium in GI tract, thus your body makes more PTH to absorb calcium from bone, causing bones to become osteopenic. renal failure need their calcium and Vit D supplementation
people get hypermagnesemia because they can't secrete it.
also have accelerated HTN through renin angiotensin system, very difficult to control, combo of accelerated HTN and high lipids, causes death.
always anemia, since kidneys make erythropoeitin, pts on dialysis, will usually receive erythropoietin but anemia is concomitant to ESRD
impaired immune functions, as well presumably because of toxins not excreted get pruritic.
all of these things are common, become osteopenic and break hip, acceprated lipids and HTN and get MI.
Hyperkalemia, potassium high enough you'll die
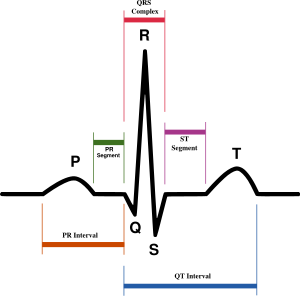
potassium is too high from changes it makes on EKG, focus on T waves..
T waves are so sharp and pointed, you don't want to sit on them:
hyperkalemia, that is an acute manifestation that potentially needs dialysis..
metabolic acidosis, in non working kidneys, is severe enough fatal needs dialysis..
fluid overload to the point of pulmonary edema, if kidney can't urinate then dialysis
pericarditis, build up in pericardial sac needs dialysis
pts with high BUN, obtunded, encephalopathic, comtaosed needs dialysis.
renal dialysis, in blood, or direct connection in the blood, venous shunt, or pertoneal, fluid swish around and come back through cath.
________________________
62 yr old pt on dialysis, returns from 4 days trip, feels very poorly (pts need dialysis every two days) he has nausea, vomiting and SOB, he has tall peaked T waves. Cr. 5.2
Hco3- is 16
metabolic acidosis
best rx is dialysis immediately..
__________________
quick recap with key words:
Eosinophils in urine = drug reaction
RBC casts= glomerulonephritis
Heavy proteinurea= nephrotic syndrome
high triglycerides= nephrotic syndrome
Radiological contrast = ATN
Urine sodium < 10 pre-renal (kidney trying to retin its plasma volume)
BUN/CR > 20 = pre-renal
 sister
sister